The release of a new set of guidelines by the American Society of Anesthesiologists (ASA) aims to reduce residual paralysis in patients following neuromuscular blockade.
The document, titled “Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade: A Report by the ASA Task Force on Neuromuscular Blockade,” offers evidence-based recommendations for the management of neuromuscular monitoring and antagonism of neuromuscular blocking agents (Anesthesiology 2023;138[1]:13-41). The ASA views the new guidelines as an important advancement in patient safety and satisfaction.
“Guidelines provide evidence-based recommendations for busy clinicians who don’t have time to read the scientific literature,” said Karen B. Domino, MD, MPH, a professor of anesthesiology and pain medicine at the University of Washington, in Seattle, the chair of the ASA Committee on Practice Parameters and a member of the task force that put together the document. “The new guidelines provide easy-to-read and easy-to-understand recommendations based upon strong scientific evidence, and will help anesthesiologists reduce the likelihood of residual paralysis and its associated respiratory complications.”
As the guideline authors discussed, inadequate recovery from neuromuscular blockade is associated with many potential adverse events, such as upper airway obstruction, reintubation, atelectasis, pneumonia, prolonged PACU stay and decreased patient satisfaction. Although residual neuromuscular blockade is usually not recognized, evidence shows that preventing its occurrence may improve patient outcomes.
Best Practice Includes Quantitative TOF Monitoring
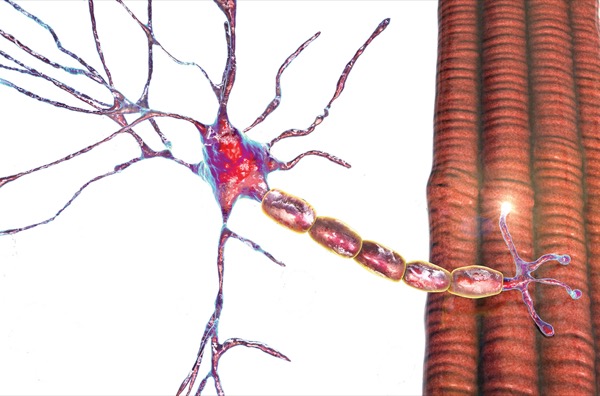
One aspect of such prevention is neuromuscular blockade monitoring, which owes its origin to peripheral nerve stimulators of the 1950s, but changed radically with the advent of train-of-four (TOF) assessment about two decades later. Although TOF was originally determined by human assessment of four thumb movements, technology has advanced to the point where monitors are now available to accurately assess these movements.
Contemporary quantitative TOF monitors offer an objective, reproducible method of measuring the TOF ratio, thereby potentially identifying residual neuromuscular blockade following surgery. By current standards, adequate recovery of neuromuscular function is defined as a TOF ratio of at least 0.9, which should be measured at the adductor pollicis muscle after ulnar nerve stimulation.
“Nearly two decades ago, experts began recommending the use of quantitative neuromuscular monitoring to ensure adequate recovery or antagonism from neuromuscular blockade,” Domino said. “However, many anesthesia providers have relied upon the use of either qualitative or clinical assessment, which they learned during their training. Unfortunately, these assessment modalities are inadequate to detect residual paralysis.”
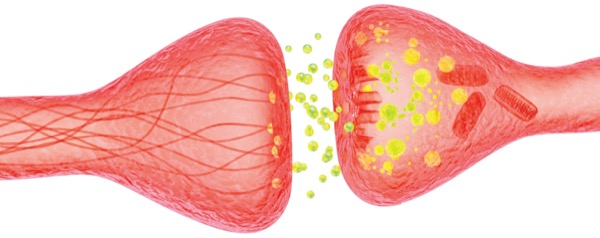
Indeed, despite the advent of novel monitoring modalities, some studies have documented incidences of residual neuromuscular blockade higher than 60% following the use of nondepolarizing neuromuscular blocking agents. Part of the issue is the pharmacologic variability between muscle relaxants and reversal agents. Furthermore, the relationship between the depth of blockade and pharmacologic antagonism is not well understood by many clinicians. As such, many clinicians use “fixed dose and blind” antagonism regimens, which often do not result in full recovery. Although the introduction of sugammadex (Bridion, Merck) has reduced the incidence of residual neuromuscular blockade compared with neostigmine, the problem has not been eliminated.
“The duration of action of neuromuscular blocking drugs varies dramatically among patients,” Domino noted. “Many anesthesiologists learned in residency that a five-second head lift or strong grip strength indicates adequate recovery of neuromuscular function. However, we now know this premise is incorrect. Studies have shown that healthy volunteers can sustain a head lift with a train-of-four ratio as low as 0.45. A train-of-four ratio greater than 0.9 is recommended prior to extubation.”
As Domino noted, the presence of four visible twitches or sustained tetanus on qualitative neuromuscular monitors is also inadequate. “Fade can’t be appreciated until the train-of-four ratio is less than 0.4,” she said.
8 Key Recommendations
Given the persistence of this problem, the ASA Committee on Practice Parameters convened a task force of anesthesiologists, epidemiology-trained methodologists and patient representatives. Together, they outlined the criteria that guided the systematic review, which comprised a search of the PubMed, EMBASE and SCOPUS databases for relevant studies published between 1990 and June 2022. The Cochrane Central Register of Controlled Trials was also queried. Eligible studies included randomized and non-randomized trials, comprising diagnostic, before-after/time series, cohort, and case–control designs.
As a result of the literature search, the expert panel made eight recommendations:
- When neuromuscular blocking drugs are administered, the panel recommends against clinical assessment alone due to the insensitivity of the assessment (strong recommendation; moderate strength of evidence).
- The guidelines recommend quantitative TOF monitoring over qualitative assessment (strong recommendation; moderate strength of evidence).
- When using quantitative monitoring, the panel recommends confirming a TOF ratio of 0.9 or greater before extubation (strong recommendation; moderate strength of evidence).
- The guidelines recommend use of the adductor pollicis muscle for neuromuscular monitoring (strong recommendation; moderate strength of evidence).
- Similarly, the guidelines recommend against using eye muscles for neuromuscular monitoring (strong recommendation; moderate strength of evidence).
- With respect to the comparative safety and efficacy of antagonist drugs, the panel recommends sugammadex over neostigmine at deep, moderate and shallow depths of neuromuscular blockade induced by rocuronium or vecuronium (strong recommendation; moderate strength of evidence).
- Conversely, the panel suggests neostigmine is a reasonable alternative to sugammadex at minimal depths of neuromuscular blockade (conditional recommendation; low strength of evidence).
- Finally, the panel recommends antagonism with neostigmine at minimal neuromuscular blockade depth when atracurium or cisatracurium is administered and qualitative assessment is used. In the absence of quantitative monitoring, however, at least 10minutes should elapse from antagonism to extubation. On the other hand, when quantitative monitoring is employed, extubation can be done as soon as a TOF ratio of 0.9 or greater is confirmed before extubation (conditional recommendation; very low strength of evidence).
As the guideline authors discussed, routine quantitative monitoring for patients undergoing neuromuscular blockade represents a shift in clinical practice, one made more challenging by the fact that monitors are not always available. Although many clinicians continue to use clinical indicators to guide decision making about patient extubation, there is no clinical test predictive of adequate neuromuscular recovery. So, there is an ongoing need to hasten the adoption of quantitative TOF monitoring to improve patient outcomes.
Education an Important Element of Implementation
Stephan Thilen, MD, MS, an associate professor of anesthesiology and pain medicine at the University of Washington, in Seattle, and Wade A. Weigel, MD, a staff anesthesiologist at Virginia Mason Franciscan Health, also in Seattle, who were co-chairs of the task force, recommended in an email to Anesthesiology News that anesthesiologists read the full article, which they said includes suggestions for implementation of quantitative monitoring. “First, each department must decide on which type(s) of monitors to make available, and it may be a good idea to allow colleagues to try different monitors and to weigh in on which ones to get. Making quantitative monitors available in all anesthetizing locations is important but not sufficient.”
Education is another important part of implementation, Thilen and Weigel continued.
“If a local champion is available to lead the implementation, this has proven helpful,” they noted. “Remind colleagues that this is a wonderful opportunity to do more of what attracted many of us to our specialty—namely, to use technology to follow pharmacology and physiology in real time. We also need reminders that there is convincing evidence that quantitative monitoring is the only approach to ensure that every patient has an adequate recovery from neuromuscular blockade.”
Domino noted that the recommendations are designed to improve clinical care by summarizing new literature for clinicians. The recommendations are not standards or absolute requirements, nor are they intended to replace local institutional policies; and they may be adopted, modified or rejected by clinicians according to clinical needs and constraints.
By Michael Vlessides
Domino, Thilen and Weigel reported no relevant financial disclosures.