CHARLOTTE, N.C.—The type of anesthesia used during endoscopic functional lumen imaging probe evaluation of the gastroesophageal junction (GEJ) can influence esophageal pressure and potentially disguise characteristics of certain esophageal motility disorders, ultimately making it difficult to achieve an accurate diagnosis, according to the results of a new study.
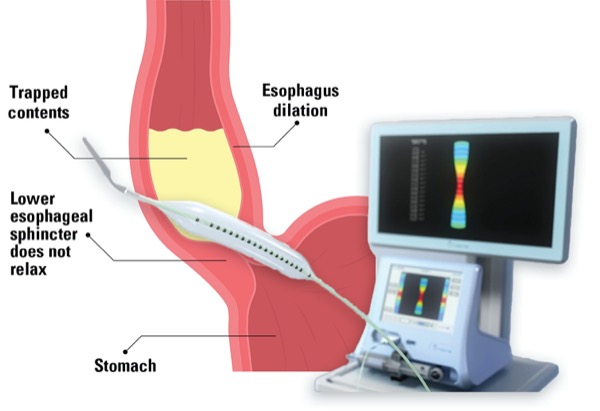
EndoFLIP (Medtronic) measures the pressure, diameter, distensibility and topography at the GEJ. “The reason we care about these measures is that they will differ depending on types of the esophageal motility disorder,” said Jennifer L. Grossman, MD, an internal medicine resident at the University of Maryland School of Medicine, in Baltimore, presenting the study at the 2022 annual meeting of the American College of Gastroenterology (abstract C0211).
In nonspastic esophageal motility disorders, such as type I achalasia, there is no esophageal motility in the body of the esophagus, so the pressure should be relatively low and the distensibility index relatively higher at the GEJ. In spastic esophageal motility disorders, such as types II and III achalasia and jackhammer esophagus, the opposite occurs.
Neuromuscular Blockade and EndoFLIP Findings
“Different anesthetics introduce different degrees of neuromuscular blockade and relax the muscles to a different degree,” Grossman said, noting that propofol induces less neuromuscular blockade than sevoflurane. Could a higher degree of neuromuscular blockade make a spastic disorder look like a nonspastic one?
The hypothesis that increased muscular relaxation could lower the pressure and raise the diameter and distensibility index measures captured by EndoFLIP initially was incidentally noted when a patient had pre-peroral endoscopic myotomy (POEM) EndoFLIP measurements taken under general sedation with sevoflurane. The measurements were vastly different from the ones from the original diagnostic esophagogastroduodenoscopy, with EndoFLIP testing done under monitored anesthesia care sedation with propofol.
Grossman and her co-investigators started to collect EndoFLIP data tandemly on patients who underwent POEM at their center between 2017 and 2022, including all patients whose sedation included both propofol and sevoflurane. The use of both agents was designed to capture an accurate diagnosis of the esophageal motility disorder under propofol sedation, then change the sedation to sevoflurane to create a more stable endoscopic surgery environment with a relaxed esophagus.
Of the 49 patients who met the criteria, 19 had type I achalasia (nonspastic), and 30 had either type II or III achalasia or jackhammer esophagus (spastic). The researchers looked at the difference in pressure measurements in the esophagus when the EndoFLIP was inflated to either 30 or 60 mm. They divided the differences into terciles and compared between diagnoses.
“In type I achalasia, the measurements correlated more with the lower tercile difference, meaning there wasn’t much of a difference in pressure whether the anesthesia was sevoflurane or propofol,” Grossman said.
But in patients with spastic achalasia, the measurements correlated more closely with the higher tercile, meaning there was a greater difference in pressure in the esophagus depending on choice of the sedating agent.
“There was a greater degree of relaxation induced by the anesthesia with sevoflurane in those spastic groups. … If you’re using a higher neuromuscular blockade anesthesia and relaxing the muscle significantly, the spastic achalasia could look like nonspastic achalasia during an EndoFLIP evaluation,” Grossman said.
“Based on this, if you have to choose between propofol or sevoflurane to diagnose an esophageal motility disorder using EndoFLIP, we recommend using propofol over sevoflurane. Likewise, choosing sevoflurane may make POEM easier since the esophagus is less spastic during the surgery.”
EndoFLIP Is Only Part of the Picture
Commenting on the findings for Anesthesiology News, Amit Patel, MD, a gastroenterologist and an associate professor of medicine at Duke University School of Medicine and the Durham VA Medical Center, in Durham, N.C., said, “This interesting study demonstrated differences in FLIP measurements acquired with sevoflurane for general anesthesia, compared to those acquired with propofol. These differences may even carry the potential for misdiagnosis of esophageal motor function.
“In the setting of limited normative and diagnostic FLIP data with sevoflurane, these findings suggest that sevoflurane ideally should not be utilized for index diagnostic evaluation for esophageal motor disorders,” Patel said. “Instead, patient selection for POEM should be thoughtfully based on appropriate diagnostic workup concordant with appropriate indications,” he added.
By Monica J. Smith
Grossman and Patel reported no relevant financial disclosures.