Patients receiving neuromuscular blocking agents during anesthesia should be carefully monitored using quantitative approaches to ensure safety and optimal outcomes, according to recently released guidelines from the American Society of Anesthesiologists (ASA) and the European Association of Anaesthesiology and Intensive Care (ESAIC).
In a joint letter to the editor published in Anesthesiology, experts from both groups highlighted the importance of the guidelines, which were based on thorough, systemic review of existing literature (Published on June 2, 2023. doi:10.1097/ALN.0000000000004630).
“The data that were reviewed by the ASA guideline committee showed that the incidence of postoperative weakness because of residual effects of the paralyzing drugs was higher than what people had expected, and was leading to more postoperative breathing complications than was realized,” Michael W. Champeau, MD, the president of the ASA, told Anesthesiology News.
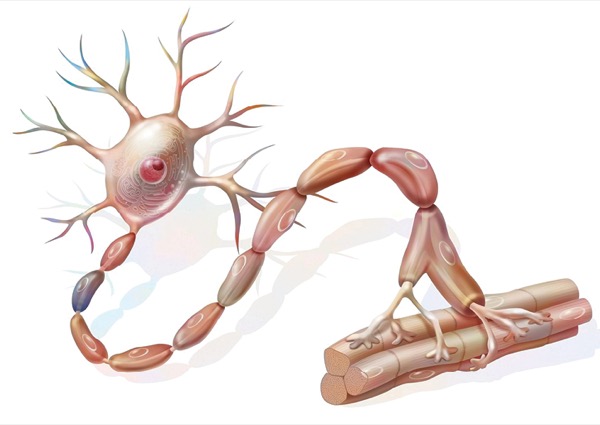
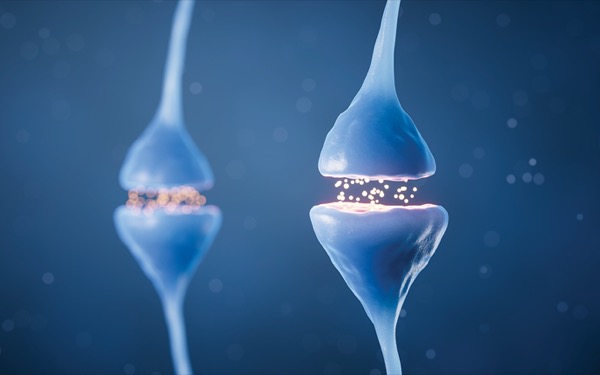
Neuromuscular blockers are commonly used in anesthesia to facilitate intubation and provide optimal conditions for surgery. Studies suggest that when patients receiving the medications are not actively monitored during surgery, the risk for postprocedure paralysis and lung problems, such as pneumonia and bronchitis, increases.
Champeau said the development of use of shorter-acting medications and a reliance on qualitative monitoring caused many healthcare professionals to feel they were adequately monitoring their patients.
“In the old days, the only available muscle relaxants were very long-acting,” he said. “All of us were in the habit of routinely giving reversal drugs at the end of the case. We could tell from the limited monitoring we had available that there was still some effect of those drugs and that patients had some degree of residual weakness or paralysis from them.
“As muscle relaxants became shorter acting, many of us often felt that enough time had gone by since the medicines had been given, and using the qualitative monitoring that we had—or using clinical signs such as watching the patient hold their head up—was sufficient to be reassured that there was no significant residual neuromuscular block,” he continued.
The data, however, told a different story.
One example comes from a recent European survey of 17,150 individuals who had received neuromuscular blocking agents. The report found that neuromuscular monitoring was not performed in more than half of patients, and that this inappropriate management increased the rate of residual paralysis and relaxant-associated postoperative pulmonary complications (Lancet Respir Med 2019;7:129-140).
Both the U.S. and European guidelines were developed to address such issues (Anesthesiology 2023;138:13-41 and Eur J Anaesthesiol 2023;140:82-94).
Key to the guidelines are a few steps, which are outlined in the joint letter:
- restructuring the clinical environment by placing quantitative monitors in all anesthetizing locations;
- employing education efforts in anesthesia departments and with individual physicians;
- providing performance feedback in the department and for individual physicians; and
- appointing a local champion who is supported by leaders.
Champeau noted that, as is true for many advances in medicine, adoption of the guidelines may take time.
“Implementation will go more slowly in lesser-resourced environments,” he said. “Education is different if you are in a 60-OR major medical center than if you are in a one- or two–OR, freestanding surgery center.”
Larger organizations, he said, often benefit from the personalized attention of manufacturers.
“If you are in a major hospital and product orders are large, you get the attention of the vendors. They send in representatives and educators to train. That is a best-practice scenario.”
Despite the challenges posed by implementation, Champeau stressed the importance of the guidelines—highlighted by the fact that both U.S. and European organizations developed their strikingly similar recommendations while working entirely independently.
“Neither organization was aware that the other was working on this,” he noted. “With COVID, we just weren’t in as much contact with one another. We thought it was remarkable that both of us came to the same conclusion.”
Much of the impetus to draft the letter to the editor was to maximize publicity in order to drive change. While implementation may take time, the effort is well worth the reward to both patients and providers.
“A lot of people may say, ‘Oh, this just isn’t a big problem,’” Champeau said. “But the data showed that in fact it is more of a problem than we thought. The guidelines are based upon the strength of the data.”
—Ethan Covey
Champeau is the president of the American Society of Anesthesiologists and a member of the board of the ASA. He is an employee, 16% owner and a member of the board of the Associated Anesthesiologists Medical Group, Inc. His wife, now retired, was an employee and a minor shareholder of Palo Alto Foundation Medical Group.