Originally published by our sister publication Pharmacy Practice News
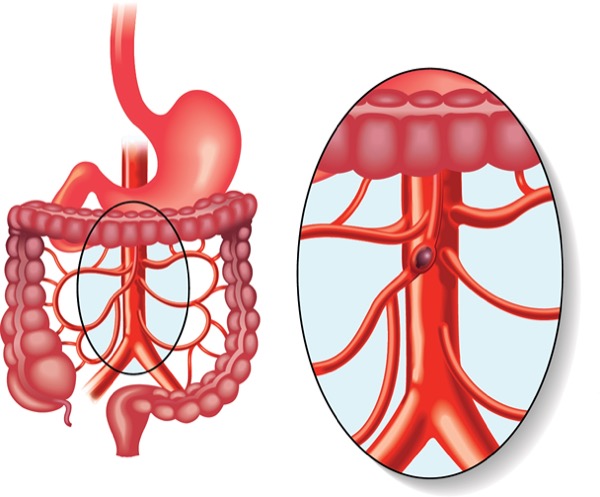
Critically ill, hemodynamically unstable patients are often treated with vasopressors, which heighten the risk for bowel ischemia. But the condition, marked by poor blood supply and intestinal damage, does not preclude the use of enteral nutrition (EN), as long as an interdisciplinary team is on board to safely guide therapy, panelists noted during the ASPEN 2025 Nutrition Science & Practice Conference, in Columbus, Ohio.
To ensure successful outcomes, the team needs to consider multiple factors, noted panelist Anne M. Tucker, PharmD, BCNSP, FASPEN, a clinical pharmacy specialist in critical care/nutrition support at The University of Texas MD Anderson Cancer Center, in Houston. “You can’t just look at one set of numbers and say, ‘oh, yeah, definitely we can do this.’ You also need to consider their vitals, vasopressor doses, their trajectory and stability.”
Dr. Tucker outlined four key steps that should be taken to determine when, and at what dose, EN should begin.
![]() Determine antihypotensive equivalent dose. Because patients in the ICU might be treated with several antihypotensive drugs, determining the cumulative impact of the agents being used is critical to prudent EN management. Two metrics are used to do this:
Determine antihypotensive equivalent dose. Because patients in the ICU might be treated with several antihypotensive drugs, determining the cumulative impact of the agents being used is critical to prudent EN management. Two metrics are used to do this:
- The vasopressor dose equivalent (VDE). Recommended by ASPEN, the VDE is calculated by multiplying the micrograms per kilogram per minute by a specific multiplier provided by ASPEN for each agent. If the VDE is greater than 12, clinicians should be cautious, using only trophic EN or holding EN until the VDE decreases below 12. However, Dr. Tucker warned that the VDE has not been validated in clinical situations (JPEN J Parenter Enteral Nutr 2022;46[7]:1470-1496).
- The norepinephrine dose equivalent (NEQ). This alternative to the VDE, recommended by the European Society for Clinical Nutrition and Metabolism (ESPEN), has been used in clinical trials to determine the optimal antihypotensive drug dosage. Similar to the VDE, it is calculated by multiplying the micrograms per kilogram per minute by a specific multiplier for each agent used provided by ESPEN. “An [NEQ] less than 0.2 mcg/kg per minute is associated with improved enteral feeding tolerance. In contrast, an NEQ greater than 0.4 mcg/kg per minute has been shown in multiple studies to predict an increased risk of gastrointestinal intolerance or adverse consequences,” Dr. Tucker explained (JPEN J Parenter Enteral Nutr 2013;37[5]:641-651; others).
![]() Measure mean arterial pressure (MAP). This hemodynamic parameter provides insight into perfusion. “Adequate perfusion for enteral feeding is defined as a MAP greater than or equal to 60 mm Hg,” Dr. Tucker said. “A MAP of less than 50 mm Hg suggests insufficient perfusion, which may lead to adverse gastrointestinal consequences.”
Measure mean arterial pressure (MAP). This hemodynamic parameter provides insight into perfusion. “Adequate perfusion for enteral feeding is defined as a MAP greater than or equal to 60 mm Hg,” Dr. Tucker said. “A MAP of less than 50 mm Hg suggests insufficient perfusion, which may lead to adverse gastrointestinal consequences.”
![]() Consider the type of vasopressor agent. A wide range of vasopressors are used in the ICU; each works at different receptors with different effects on GI perfusion, MAP and cardiac output. Each agent’s effect on these factors must be considered before EN is initiated, Dr. Tucker noted, adding that norepinephrine and vasopressin are often favored in ICU patients with septic shock due to their place as first- and second-line treatments within the Surviving Sepsis Campaign guidelines. Digging a bit deeper, she offered the following added medication tips:
Consider the type of vasopressor agent. A wide range of vasopressors are used in the ICU; each works at different receptors with different effects on GI perfusion, MAP and cardiac output. Each agent’s effect on these factors must be considered before EN is initiated, Dr. Tucker noted, adding that norepinephrine and vasopressin are often favored in ICU patients with septic shock due to their place as first- and second-line treatments within the Surviving Sepsis Campaign guidelines. Digging a bit deeper, she offered the following added medication tips:
- Dobutamine, epinephrine and low-dose dopamine can increase GI perfusion, while high-dose dopamine, norepinephrine, phenylephrine and vasopressin decrease GI perfusion.
- Epinephrine, norepinephrine and phenylephrine increase MAP.
- Dobutamine, epinephrine and norepinephrine increase cardiac output.
![]() Order lab tests. Some laboratory values are associated with bowel ischemia, including lactate, base deficit and lactate dehydrogenase. These assays can help assess a patient’s acid–base status and the severity of ischemia. However, “the tests are nonspecific, because each can be abnormal in other disease states and conditions,” Dr. Tucker said. This is why laboratory assessments such as the ones cited above “are not the only piece(s) of information used to determine the appropriateness of enteral feeding in hemodynamic instability.”
Order lab tests. Some laboratory values are associated with bowel ischemia, including lactate, base deficit and lactate dehydrogenase. These assays can help assess a patient’s acid–base status and the severity of ischemia. However, “the tests are nonspecific, because each can be abnormal in other disease states and conditions,” Dr. Tucker said. This is why laboratory assessments such as the ones cited above “are not the only piece(s) of information used to determine the appropriateness of enteral feeding in hemodynamic instability.”
Stephanie Dobak, MS, RD, LDN, CNSC, of the Jefferson Weinberg ALS Center, in Philadelphia, who was the session moderator, also noted that monitoring patients’ lactate, electrolytes, renal function, liver function, arterial blood gases and glucose levels can play a role in determining whether initiating EN is appropriate.
“If lactate is elevated due to poor perfusion, initiating EN too early may exacerbate the metabolic stress or worsen gut ischemia, though there are insufficient data to support this,” Ms. Dobak said. “Severe electrolyte imbalances (especially hypokalemia, hyponatremia or metabolic acidosis) and altered serum blood urea nitrogen, creatinine, liver function tests, arterial blood gases and glucose levels often highlight instability. If trending in the wrong direction, these labs may suggest not initiating or decreasing EN provision.”
Further Considerations
In 2022, ASPEN issued guidelines on nutrition indications (JPEN J Parenter Nutr 2022;46[7]:1470-1496). The guidelines recommend assessing patients for initiation of EN within 48 hours of vasopressor administration, with a preference for gastric feeding. Dr. Tucker noted that signs/symptoms of abdominal pain, distension, high nasogastric output and high gastric residual volume should also be monitored, and if symptoms indicate that the GI tract is not functioning correctly, EN should be delayed. (For an ASPEN practice tool on these and other considerations for starting EN in critically ill patients, visit bit.ly/4czecdm.)
Due to the complexity of determining the appropriate time to initiate EN in hemodynamically unstable patients, “all medications and nutrition plans should be discussed on daily interdisciplinary rounds. This allows individual team members to collaborate and bring together our strengths to make the best decision,” Dr. Tucker said. In particular, “pharmacists are key to this process because they know vasopressor medications, their adverse effects and their complications. Based on the types and doses of vasopressors in use, pharmacists can provide the medical team with insight into situations where enteral nutrition may be problematic.”
Ms. Dobak agreed. “The decision to provide EN for hemodynamically unstable patients requires an interdisciplinary collaboration,” she said. “While the physician makes the ultimate call, the pharmacist provides insight into pressors and other concurrent medications, the bedside nurse gives awareness of the patient’s minute-to-minute trajectory and abdominal exam, and the dietitian offers expertise on different EN formulas and GI access.”
Ms. Dobak reported no relevant financial disclosures. Dr. Tucker is a consultant to UpToDate Inc.

Please log in to post a comment
This is a fundamental issue. Still, it looks like there is no solution at the moment. I disagree that we need a team to resolve. We probably need a validated tool or score that will help in deciding. Thank you.